The climate emergency continues to bear consequences for people’s health, and the hardest hit places are often those least responsible for the emissions that fuel it.
In Kenya, extreme climate conditions have led to three concurrent disease outbreaks—malaria in Baringo and Turkana counties, which have experienced heavy rains, and measles in Marsabit county. Residents of these arid or semi-arid regions often struggle to access health care due to the long distances to reach health centers, the high cost of transport, and the difficult terrain.
All three regions also suffer from serious shortages of qualified health workers. This situation has prompted Doctors Without Borders/Médecins Sans Frontières (MSF) to launch three simultaneous responses in Kenya.
Turkana West, northern Kenya
At the malaria peak in September, 8 out of 10 people in Turkana West tested positive for the disease. MSF launched a response in 16 villages in the Kalobeyei area, treating 1,909 children and adults for malaria, as well as providing 2,992 outpatient consultations and extra health staff. MSF sent additional staff to the Ngiitakito dispensary in Lodwar to improve infection prevention and control measures for better management of malaria cases.
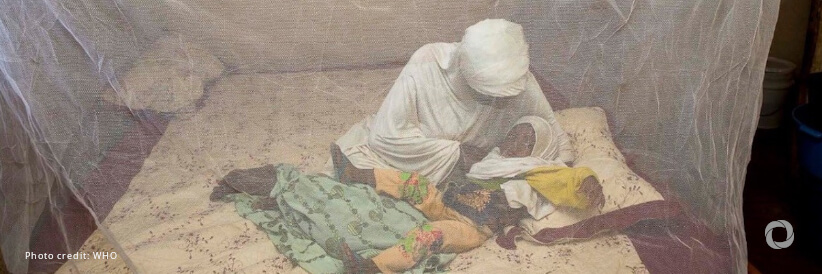
The MSF team in Turkana West also provided mosquito nets to households that did not have them. “This area had malaria prevention interventions in the recent past,” said MSF emergency coordinator Lili-Marie Wangari. “We are helping to identify households that were not reached during the last net distribution carried out by health authorities.”
As most malaria patients are between 5 and 15 years old, the team also installed 350 mosquito nets in a local boarding school.
Marsabit, northern Kenya
Following a measles outbreak in August in Illeret, Marsabit county, an MSF team worked with the Ministry of Health to carry out mass vaccinations targeting children from 9 months to 15 years old. Working with 12 community health promoters, they vaccinated a total of 9,874 children to protect them against the disease. During the campaign, MSF staff also identified children with complicated forms of measles, provided them with treatment, and referred patients in need of specialized care to health facilities.
In Illeret, 12 community health promoters who live within these communities have been instrumental in the mobilization of the community to expand its reach.
“Beyond access to health facilities, mechanisms for reporting public health events within these communities by community members and volunteers are crucial for early detection of diseases and linkage to facilities,” said Wangari.
During the three emergency responses, MSF teams treated 4,944 patients for malaria and provided other outpatient medical consultations to more than 8,000 people. More than 9,800 9, children between 9 months to 15 years old were vaccinated for measles and 26 new measles cases were identified and managed.
Over 1,000 children and 386 pregnant and breastfeeding women were screened for malnutrition, and 249 children were found to have moderate acute malnutrition in addition to 158 with acute malnutrition. The response involved the work of 38 community health promoters and volunteers to support community-level disease detection.